Move to Improve making things healthier and safer by getting people moving
Research shows that getting people moving within 24 hours of being in the hospital is important.
Early mobilization is part of the picture. But how do you know if people continue to get moving, and if they're moving often enough to maintain their strength, and with increasing challenges to improve their strength?
That's why health professionals at the Grace Hospital were asked to do a pilot project on early mobility. A 36 bed medical unit where the average age is 80 (3 South) was chosen for the pilot.
An interdisciplinary team who attended the Dorothy Wylie Health Leaders Institute (Monique Wichenko, Carly Proctor, Rob Gibson and Eve Omar) started developing the work that would eventually become the pilot program Move to Improve. Work began on these complex issues in 2013.
"We have a culture that when we're in hospital, we need to rest," says Mary Anne Lynch, Program Director for the Regional Medicine Program and Grace Hospital Medicine Program. "That's part of it. We do need rest. But we also need to balance resting with mobility and activity so patients don't lose functioning. We need patients to maintain their functioning and/or improve functioning while in hospital so they can return back home."
Research shows that one-third of people who are older who aren't mobilized early in hospital will lose ability to do one or more activities of daily living. Research also shows that less than 20 per cent of people are mobilized regularly in hospital.
This means with a hospital stay, a person's ability to function in their daily lives can be negatively impacted.
That's why this pilot is so important. Early mobility has proven benefits in improving health outcomes. It helps patients return to their previous ability to function, and can help decrease the duration of delirium and risk of depression. It also means patients go home sooner, and spend less time in the hospital.
The goal was to create an evidence-based strategy to provide safe, early and progressive mobility for all patients during their time as inpatients at Grace Hospital on unit 3 South. Looking at mobility as a shared responsibility of the interdisciplinary team, also including patients and their families by helping them understand the need for, and the value of early mobility while hospitalized was also part of the approach.
Each person's ability - given their situation - was a part of the factor in their movement goals. If a person wasn't able to get up and walk, for example, health care providers would ensure that their limbs were manipulated. There are gradual stages of movement - sitting up in a chair, getting to the washroom, and walking around the unit with assistance and without.
Revamping an existing form was key to enabling everyone on the health care team to monitor and document each person's mobility. The Mobility and Toileting Routine document was also posted to enhance accessibility and transparency around a person's mobility.
This is important, says Lynch, because documentation is always a challenge. It's hard to know if patients are actually mobilizing regularly throughout the day and their hospital stay if it isn't documented.
"What we learned with this pilot is that it's a unit team's responsibility to mobilize our patients, not one person's job. The physiotherapist can provide daily treatment, but maintenance of the patient's treatment care plan is a team effort that involves nurses, health care aides and the patient," says Lynch.
There was an education component to the pilot supported by Rianna Bettencourt, Program Educator. Management and staff were educated about the research, the benefits and the project, but also patients and their families needed to be made aware of the importance of early and regular mobility while in hospital.
"We found out that family members and friends were supportive and willing to help get their loved ones up and moving," says Lynch.
Patient outcomes for the pilot were exciting. Documented frequency of mobilization in the care plan went from five per cent to 39 per cent. Distance of mobilization documentation in the care plan improved from 13 per cent to 39 per cent.
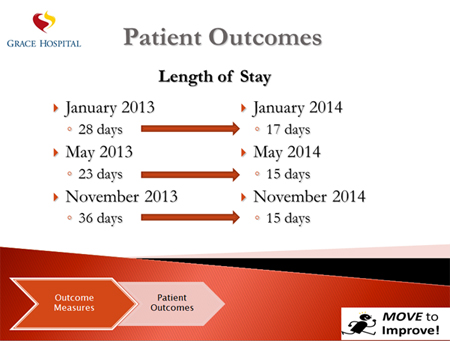
While many initiatives to decrease length of stay have been implemented within the Medicine Program at Grace Hospital, it appears there is a connection between early mobility and further reductions in length of patient stay.
One of the biggest surprises from the pilot was a 50 per cent reduction in falls on the unit.
"We felt that this was absolutely attributable to Move to Improve," asks Lynch. "How do you get patients and family and the team to realize if you want to decrease the risk of falls in hospital, patients shouldn't stay in bed, they actually need to get up and mobilize regularly mobilizing and activity is good for all patients in hospital, but if you are concerned about risk of falls in some patients, encourage regular mobility . . . it helps increase strength, confidence and safety."
Managers who support this effort and unit staff champions can help ensure early mobility is included consistently in the plan of care. In addition to the project team, the 3 South champions are Tess Simbulan, Michell Towes, Karen Cannell-Jamieson, and Kristy McIntosh.
"Unit champions have the ability to influence the culture on the unit," says Lynch. "Champions from different disciplines can speak to the importance of early mobility and help create clear outcomes."
Ceiling markers that identify distance in metres were added by Leslie Dryburgh, Clinical Nurse Specialist-Geriatrics during the pilot period help provide visual cues for both patients and their health care providers. But they also help with care planning, says Lynch.
"The markers are helpful for the patient and their family and the team to actually visualize and quantify the distance that the patient can walk, and the improvements made day to day. This is also important when we are planning for discharge she says.
A rollout for Move to Improve throughout the Grace Hospital is currently in the planning stages.