Responsive, practical tool helps introduce change
Experience Change model used at HSC Winnipeg to introduce change in manager hours
The challenge: two managers in the adult emergency department had similar hours. The proposed change: change the expectation for hours so that there was greater coverage and presence by a manager.
The proposed change represented quite a shift. To have a clinical manager - who wasn't a nursing supervisor - with expectations of working in the evening was a radically new concept.
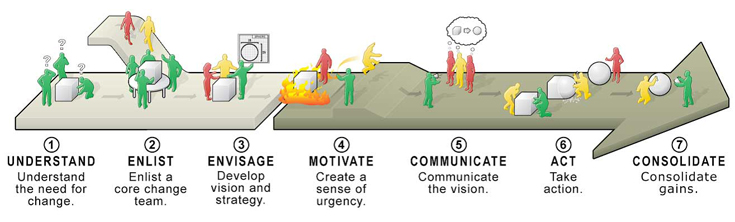
Enter Experience Change, a change management model that Health Sciences Centre, Winnipeg (HSC) used, with two key phases and seven stages. The model acknowledges change is a process, not an event. Communication and a commitment to change at an individual and organizational level is what makes change happen, and stick.
It started with conversations that answered the big question . . . why the change was necessary. Further discussion included clear expectations and boundaries, and included the support of Kathy Derksen, the Chief Nursing Officer at HSC.
"There is a difference between understanding and acceptance," says Carol Legare, Director of Patient Services, Emergency Program at HSC. "These people may report to me but they are also my friends and colleagues. It was important to reinforce intention."
And part of the way to look at honouring the relationships and the need for change at the same time was to do an exercise that looked at "in your perfect world". That allowed the people impacted by the change to provide their perspective on how to best make this transition.
It's also why the change in hours happened in two phases. What resulted is a manager who starts at 0700 and works until 1500 and another who starts at noon and works until 2000.
Plan, Do, Study, Act . . . four key elements that are continuously revisited when considering implementing change. Timing is a big factor, notes Legare, who says a critical initial question needs to be if given other variables, it's the right time for the change.
Communication to the rest of the campus about this change, how it would unfold and the benefits of it - to help facilitate patient flow - was clear.
The biggest positive impact of this change is the capacity to resolve issues at the ward level, and enhanced communication. Staff morale has also improved, thanks to having a manager available to talk.
"The model helped us know when to evaluate and when to rejig. It is a responsive change model that is practical and user-friendly," says Legare. "Anybody can use this for any level of change. It provides a unified, consistent way of going through things."