Infection Prevention & Control
The Winnipeg Regional Health Authority’s Infection Prevention & Control (IP&C) Program is dedicated to preventing infections for all individuals requiring care in our region. Infection Prevention and Control staff supports all WRHA hospitals and community facilities as well as partner organizations and members of the community.
→Always follow Routine Practices at all times with all patients/residents/clients (PRC), regardless of their diagnosis
→Measles (rubeola) is an acute, highly communicable viral infection (one of the most highly communicable diseases in humans). Also known as “Red Measles”
- Not to be confused with rubella (“German Measles”)
→Initial Symptoms can include:
- Prodromal fever (> 38.3° C – oral)
- Cough
- Coryza (runny nose)
- Conjunctivitis
- Malaise
- Anorexia
- Koplik spots: A symptom specific (pathognomonic) to measles, Koplik spots are small (1mm) bluish white spots which may be seen on the oral mucosa and may appear 2 to 3 days after the onset of symptoms. These spots are often confused with other lesions in the mouth. Their suspected presence is an unreliable marker of measles.
→Rash Red maculopapular rash appears 3-7 days after initial symptoms or 14 days after exposure. Measles rash appears brown or red and blotchy on white skin but may be hyperpigmented or harder to detect on black or brown skin.
IF A PERSON RECEIVING CARE HAS SYMPTOMS COMPATIBLE WITH MEASLES
- Implement Airborne Precautions immediately:
- Tell symptomatic person and anyone accompanying them to perform hand hygiene and put on a medical mask
- Place symptomatic person and anyone accompanying them into an airborne isolation room (AIR) as soon as possible. A single room with the door closed may be used if and AIR is not available.
- Minimize time in the waiting room
- Only health care workers (HCWs) with presumptive immunity1 to measles should provide care to patients with suspect/confirmed measles due to increased risk of transmission of measles to susceptible individuals
- Non-immune, susceptible staff may only enter the room in exceptional circumstances (i.e., no immune staff are available and patient safety would be compromised otherwise)
- All HCWs regardless of presumptive immunity to measles are to wear a fit-tested, seal-checked N95 respirator when providing care to someone with suspect or confirmed measles
- Notify your site/area/program Infection Control Professional
- Test:
- For suspect cases of measles, preferred specimen is a nasopharyngeal (NP) swab (flocked swab in viral/universal transport medium) for measles virus PCR. A NP aspirate is acceptable AND
- Collect blood for serologic testing (measles IgG and IgM). Include date of onset of both fever and rash. Do not send serology alone; nasopharyngeal swab is required
- Send NP and serum to Cadham Provincial Laboratory.
- If you have access to EPR:
- Implement Airborne Precautions for persons with “RESP RISK” EPR Health Issue flag
- Specific dates for precautions are indicated in the Description Box of the Health Issue
- Consult Infectious Diseases for high-risk contacts (i.e., immunocompromised, pregnant, and/or non- immune needing IVIG)
- Manitoba Health requires same day reporting for measles cases. All probable and confirmed cases must be reported on the same day to WRHA IP&C on weekdays, and Manitoba Health on weekends/evenings/nights:
- During business hours: On-site IP&C staff will complete the Clinical Notification of Reportable Diseases and Conditions form on behalf of the diagnosing physician if promptly notified
- During weekends/evenings/nights: Contact the Manitoba Medical Officer of Health on call at 204-788- 8666. Complete the Clinical Notification of Reportable Diseases and Conditions form and fax to Manitoba Health at 204-948-3044
- Review PRC immunization histories and update vaccinations as required
- If required, contact Occupational and Environmental Safety and Health (OESH) for concerns related to possible staff exposures to measles
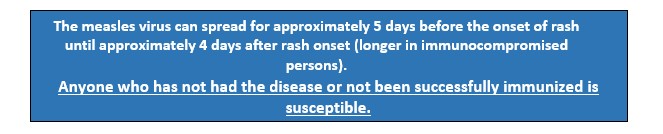
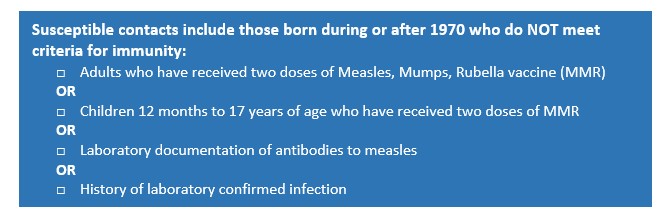
1 Criteria for immunity for HCWs: HCWs are considered immune to measles if they have laboratory confirmed evidence of either immunity or disease or a history of two doses of a measles containing vaccine after their first birthday. HCWs who do not meet these criteria should receive one or two doses of vaccine as required. Non-immunized HCWs who are exposed to measles who are found not to be immune will be furloughed from days 5-21 post exposure.
Management of Measles Contacts
- Implement Airborne Precautions for any person receiving care who is a susceptible contact to measles:
- From day 5 after their first exposure to day 21 after their last exposure regardless of post- exposure prophylaxis.
- Ensure eligible contacts receive immunoprophylaxis unless contraindicated.
Resources:
- Routine Practices
- Airborne Precautions
- Measles Specific Disease Protocol
- Clinical Notification of Reportable Diseases Form
- Infectious Rash IP&C Measures Algorithm
- Managing Measles Presentation in a WRHA ER/UC setting
- Managing Measles Presentation in a WRHA clinic setting
- Manitoba Public Health Fact Sheet
- Manitoba Health Measles, Mumps, and Rubella (MMR) Vaccine Eligibility
- PHAC Measles and Rubella Weekly Monitoring Reports -2025
